
Nursing assessments are critical to the job of being a nurse, and there are several different types of assessments that nurses need to be able to perform. They may be broad in scope or more focused on one body system or issue.
Let’s go over different types of nursing assessments with some expert tips along the way!

While the nursing process includes nursing assessments, it is much more than that. It also includes four other steps that enable the nurse to successfully care for patients and ensure effective care.
As a nurse, the types of assessments you perform will change based on the reason for the patient coming in and the information that any previous assessments have provided.
This is one of the most comprehensive nursing assessments to conduct and is usually done when a patient first arrives on an inpatient nursing unit. (A different assessment will be completed in the emergency department, which is often the first contact the patient has with medical staff. More on that soon.)
While a head-toe-assessment will be completed at routine intervals, the initial admission assessment will be more detailed and performed only once. The key 🔑 difference is that there will be more background questions during an admission assessment so that we can establish a baseline and ensure their living environment is safe.
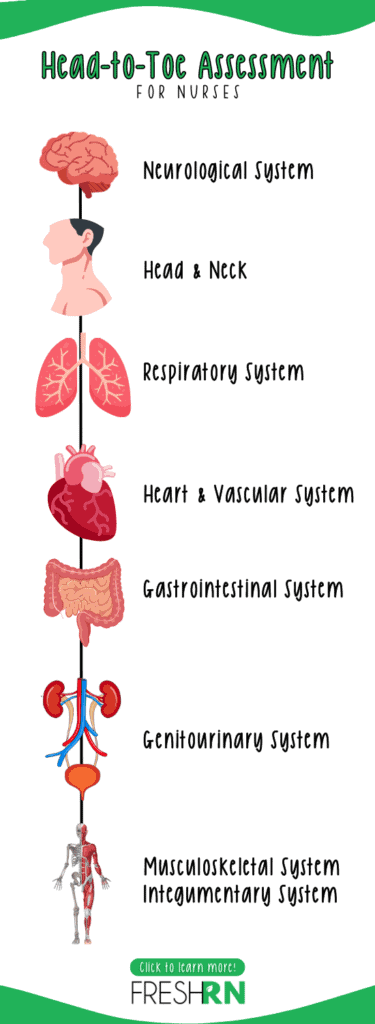
The exact order of the assessment is up to the individual nurse, but many nurses prefer to go from top to bottom (or head to toe!). If your nursing assistant has not taken a set of vitals already, this would be a great time to do so.
Here’s a basic checklist head-to-toe nursing assessment checklist:
This assessment is basically identical to the previous assessment, except you won’t be asking all of those psycho-social home assessment questions repeatedly.
Pro-tip ➡️ Perform your assessment the same way each time, like a golf swing. This will prevent you from missing steps and enable you to engrain the process faster into your muscle memory. To check out my inpatient cardiac patient assessment routine, click here and I’ll email you a PDF.
Focused 🔎 assessments are nursing assessments that target the specific body system where the patient demonstrates a problem, disorder, or concern. This can relate to one or multiple body systems. You’ll most often see these performed in emergency departments when a patient presents for a specific issue or on a regular nursing unit when a change occurs (like a new neuro change).
The goal is to identify and address a specific issue, not a comprehensive medical evaluation for all possible factors that could be impacting a person.
Nurses should use their best clinical judgment to determine which focused assessments pertain to their patient based on a previous head-to-toe assessment and input from the patient. (Typically in an urgent situation for inpatients and most emergency department patients).
Nurses can perform focused assessments in any of these areas:
While completing a focused assessment, a nurse should ensure the patient remains stable overall and not become overly fixated on that one aspect of the assessment. For example, if a patient complains of eye pain but shortly thereafter begins complaining of shortness of breath, the nurse should not wait to address the shortness of breath until the eye assessment and interventions are complete. Pivot as the clinical picture evolves and requires it.
Don’t be discouraged. It takes time to develop nursing critical thinking skills, especially in urgent situations that require focused assessments.
Patient emergencies happen in all areas of the hospital. They most often occur in the emergency room and the intensive care unit, but they can happen in any unit.
These assessments occur when something happens suddenly (like when the patient codes!), and we need to assess the patient as quickly as possible to implement interventions quickly.
Nurses perform emergency assessments when a patient experiences a cardiac or respiratory code or if a patient appears to be in significant distress, and the acronym ABCCS is extremely helpful

Here’s what the acronym stands for:
Once the patient stabilizes, the nurse may discontinue emergency assessments and transition to an initial or focused assessment, depending on the situation.
Patients on the medical-surgical unit may be preparing for a surgical procedure or recovering from one. Or they may have an illness that requires close monitoring by a med-surg nurse to watch for any changes in their condition or the need for a higher level of care.
Every shift, a med-surg nurse must complete a head-to-toe assessment and also after any changes (like a code or if the patient went to surgery and came back). This head-to-toe nursing assessment aims to alert nurses to anything that may indicate a problem for the patient. It’s imperative to do this regularly (most policies say once per shift and with changes) so the providers and nursing staff know how the patient is doing continuously and detect changes faster.
It is a bit more abbreviated than an admission head-to-toe assessment, as previously described. While your routine skin assessment does not need to be quite as thorough, you will want to check the following additional items:
I dive deep into med-surg assessments in this course.
ICU nursing assessments are very similar to but very different from a general head-to-toe assessment because they’re more detailed due to the critical nature of the care the patient needs. You’ll do this type of assessment for each patient when you come on shift.
This nursing assessment is very similar to the med-surg patient assessment, however it includes more detail. Instead of a quick neuro check, you’ll do a more detailed version. Instead of a quick look at the skin, your patient will likely have multiple wounds or devices inserted into their skin (like a central venous catheter) that are at higher risk. Instead of 1-2 issues going on, you may have 3-5+ that require frequent management and physician collaboration.
Here is my ICU patient assessment routine, regardless of their admission diagnosis.
We outline nursing assessments of general ICU patients in this course. We discuss neuro ICU nursing assessments in depth in this course, and cardiac ICU nursing assessments in this course.
Here’s a detailed example of a nursing assessment for a patient admitted to a hospital with shortness of breath and a history of congestive heart failure (CHF):
Subjective Data Collection
Chief Complaint: The patient reports experiencing increased difficulty breathing over the past two days, especially when lying flat. The patient describes the shortness of breath as worsening with minimal exertion.
Health History: The patient has a history of congestive heart failure diagnosed five years ago, hypertension, and type 2 diabetes. Medications include Lisinopril, Metformin, and Furosemide.
Symptoms Review: The patient mentions occasional chest discomfort, fatigue, and an increase in leg swelling. The patient denies any recent fever, cough, or change in sputum color.
Lifestyle and Daily Activities: The patient reports limited physical activity due to fatigue and dyspnea. The patient lives alone and expresses concerns about the ability to manage daily activities and medication adherence.
Emotional and Mental Health: The patient expresses anxiety about the current health status and the impact of worsening symptoms on independence and quality of life.
Objective Data Collection:
Vital Signs: Blood pressure 160/90 mmHg, heart rate 102 bpm, respiratory rate 22 breaths/min, oxygen saturation 89% on room air, temperature 98.6°F (37°C).
Physical Examination:
Cardiovascular: Heart sounds include a third heart sound (S3 gallop). No murmurs detected. Peripheral pulses are palpable but diminished in the lower extremities.
Respiratory: Bilateral crackles heard at the lung bases. Use of accessory muscles noted during breathing.
Edema: 2+ pitting edema observed in both lower extremities up to the mid-calf.
Skin: Cool and pale extremities. No rashes or ulcers observed.
Diagnostic Tests:
Chest X-ray shows pulmonary congestion.
Echocardiogram pending to evaluate ejection fraction and heart structure.
Blood tests reveal elevated B-type natriuretic peptide (BNP) levels.
Based on the subjective and objective data collected during the nursing assessment, the nurse identifies several key nursing diagnoses, including impaired gas exchange related to pulmonary congestion, decreased cardiac output associated with CHF, activity intolerance related to dyspnea and fatigue, and anxiety related to health status.
The nurse then proceeds to the planning phase, setting goals to improve oxygenation, enhance cardiac function, increase activity tolerance, and reduce anxiety, with interventions tailored to address these issues. These may include administering prescribed medications, monitoring vital signs and oxygen saturation, providing supplemental oxygen, educating the patient on energy conservation techniques, and offering emotional support. The care plan is implemented with continuous evaluation to adjust interventions based on the patient’s response.
Physicians round on patients once every 24 hours (and more often if necessary), and nurses are at the bedside the other 23 hours and 20 minutes. The medical team relies on the nurse to be able to accurately assess the patient, and determine a baseline, and reassess with any changes. They trust that the RN will notify them with changes in status and need. Nursing assessments enable the RN to be able to know how the patient is doing and if changes occur in a systematic manner. This is imperative for patient safety.
The scope of a Licensed Practical Nurse (LPN) or Licensed Vocational Nurse (LVN) involvement in assessments can vary significantly depending on the state’s Nurse Practice Act, the healthcare setting, and the policies of the employing institution.
LPNs typically perform focused assessments rather than the comprehensive assessments that Registered Nurses (RNs) are trained to conduct. A focused assessment by an LPN might involve collecting vital signs, gathering specific health information related to the patient’s presenting problem or ongoing care needs, observing the patient’s condition, and reporting findings to an RN or a healthcare provider.
LPNs are skilled in identifying changes in a patient’s condition and can perform various tasks, such as:
– Measuring and recording vital signs (blood pressure, pulse, respiration, temperature)
– Monitoring and reporting changes in patient symptoms or behavior
– Performing basic physical examinations, such as inspecting the skin for wounds or checking for edema
– Gathering health history information pertinent to the patient’s immediate care needs
It’s important to note that while LPNs can collect data and contribute to the assessment process, the interpretation of assessment data, the formulation of nursing diagnoses, and the development of the overall care plan are typically responsibilities reserved for RNs or advanced practice nurses, depending on the complexity of the patient’s condition and the regulations of the jurisdiction.
To understand the specific tasks LPNs are permitted to perform in the context of patient assessments, it’s essential to refer to the local Nurse Practice Act and guidelines provided by the state nursing board, as these define the legal scope of practice for nurses at different levels of licensure.